A Post-marketing surveillance study of chronic wounds treated w native collagen
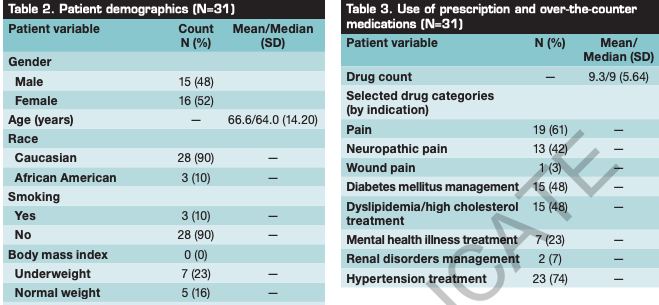
Abstract: Chronic wounds (ie, wounds that fail to progress through a normal, orderly, timely sequence of repair) continue to pose significant clinical and economic burdens. A prospective, descriptive, 3-week post-marketing surveillance study was conducted across 3 wound care centers in the United States to evaluate the effectiveness of a collagen calcium alginate dressing on chronic wounds in conjunction with standard care (SC) practices (eg, offloading, debridement, compression) to support healing. Eligible participants had to be >18 years of age, have at least 1 chronic wound, and no known sensitivity to collagen. Demographic characteristics were recorded at the screening visit on case report forms. At each visit, wound-related pain was assessed using the Visual Analog Scale along with wound characteristics including size (using digital planimetry), wound exudate (minimal, moderate, heavy), and odor (none, mild). Participants were monitored for adverse events as well as infection based on signs and symptoms in and around the local wound bed, the deeper structures, and the surrounding skin. An intention-to-treat approach was used for all analyses. If an observation was missing, the last observation carried forward principle was used. For wounds that healed, pain and exudate were set to 0 (no pain/exudate) at visit 4. Descriptive, paired t-tests and the Wilcoxon signed rank test were used to analyze the data. Of the 31 participants (15 men, 16 women, mean age 66.6 years), most (13, 42%) had a diabetic foot ulcer or venous leg ulcer (10, 32%); the median duration of all wounds was 148 days. Thirty (30) patients completed the study. The mean number of comorbidities was 10.6 ± 6.3, and patients used a mean of 9.3 ± 5.64 prescription or over-the-counter medications. For all wounds combined, the mean wound area was 4.8 ± 8.38 cm2 at baseline. At week 3, a decrease in wound area of 38.1% was noted (median: 45% ± 42.54; P = .006); 3 wounds healed completely. The change in wound exudate level from visit 1 to visit 4 was statistically significant (P = .006). No adverse events or infections occurred. In this population, the use of etiology-appropriate SC and a collagen calcium alginate dressing resulted in a decrease in wound area after 3 weeks of care. Longer-term studies to confirm these observations and controlled clinical studies to compare the effects of this dressing to other nongauze dressing treatments are needed.
A-Post-marketing-surveillance-study-of-chronic-wounds-treated-w-native-collagen